What To Know About Vaginal Atrophy And Its Treatment
What to know about vaginal atrophy and its treatment
“Be happy with what you have while working for what you want.”
– Helen Keller
Vaginal atrophy post menopause is an age-related condition. Women are more subjected to age-related changes because of the reproductive system. However, vaginal atrophy is not exclusively post menopause. Estrogen is a hormone that increases and decreases ever since menarche. Estrogen is what makes a woman. Vaginal atrophy post menopause affects the urinary system too, as it is intimately related to the reproductive system with regard to both location and evolution.
What is vaginal atrophy?
- It is the loss of thickness and tone of the vaginal muscles and thinning of the lining.
- As a consequence, the vagina loses its elasticity and contracts, and also loses its capacity to secrete the usual lubrications. The net result is a painful sexual experience or dyspareunia.
What is the extent of incidence of GSM?
- It is very difficult to have an estimate with any credibility, as most women prefer to let it pass rather than seeking medical help.
- This is because of the lack of awareness that their symptoms are related to climacteric, which requires medical assistance.
What are the associated symptoms?
- Vaginal dryness, burning, pruritus or itching, discharges, dyspareunia or painful intercourse, and slight bleeding post physical relation are some of the symptoms.
- Urinary symptoms accompanying vaginal atrophy are dysuria or painful urination, burning sensation during urination, poly urea or frequent urination, and urinary incontinence.
- Psychological symptoms are being unattractive, inadequacy, and depression in case of extreme vaginal atrophy post menopause.
What are the factors likely to increase vaginal atrophy?
- The major factor is, of course, climacteric.
- Smoking reduces blood circulation to the vagina.
- Smoking reduces the effectiveness of minimal estrogen.
- Certain medications like contraceptives and breastfeeding.
- C-section births also play a role. It is observed that women who never had normal deliveries have enhanced chances of GSM.
- Sexual abstinence, which is due to the loss of vaginal circulation during the act.
- Diabetes or Sjögren’s syndrome, which is an autoimmune condition that destroys all fluid secreting glands in the body.
How is vaginal atrophy post menopause diagnosed?
- The doctor, besides taking medical history, conducts a physical examination of the pelvic organs to ensure that no abnormalities like prolapse of uterus, bladder, or rectum are present.
- The physician may check whether the patient has any urinary complains, sometimes eliminating other conditions that produce similar symptoms.
- Vaginal acid balance is also checked. It involves either collection of vaginal fluids and testing or introducing a paper that changes its color depending on the acidity of its ambience.
What are the available treatment options for vaginal atrophy?
- A permanent cure is improbable, but also, future in the medical field is unpredictable.
- Hormone replacement treatment of menopause has already been discontinued, as the risks are far more than the success rate.
- Topical moisturizers and lubricators help. Moisturizers sustain vaginal moisture for longer.
- Natural vegetable oils are used as lubricants. The risk of allergic reactions is present in this option for treatment of vaginal atrophy.
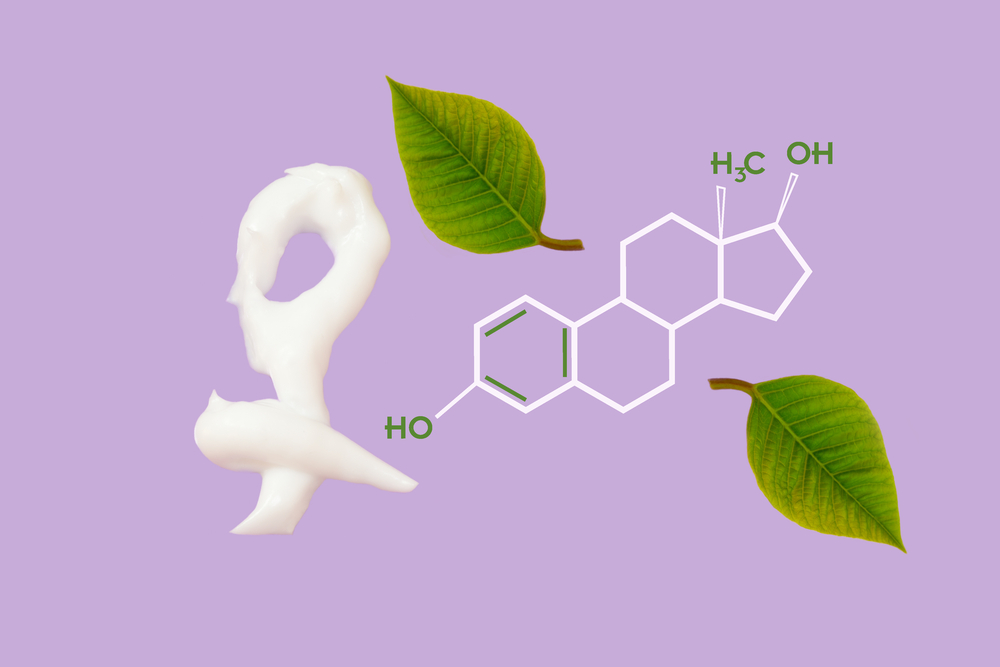
- Application of estrogen as cream, drug eluting rings, and tablets are effective treatments to vaginal atrophy. Higher concentrations run the risk of systemic effects.
- Estrogen creams are used as vaginal atrophy treatments daily for about three weeks and subsequently, reduced to one to three times a week.
- Regular sexual activity increases vaginal blood circulation with attendant benefits, acing as one of the treatments for vaginal atrophy.
- Another promising treatment for vaginal atrophy is the local androgen treatment. Vagina was considered as an organ unaffected by androgens. Research in recent times in immunohistochemistry has indicated that testosterone has both indirect and direct roles to play on the vagina. However, these researches are still in progress.
What do the investigations of SERM suggest?
- Recent researches on SERM or Selected Estrogen Receptor Modulators are considered promising. The investigations were intended to find remedies for breast cancer.
- Tissue-selective estrogen complexes or TSECs is paired with estrogen by SERM and researched for their potential to treat menopausal syndromes, vulvovaginal atrophy, and for breast and endometrium protection. They need continued research, however.